The healthcare industry is evolving rapidly, and with it, the laws governing it are becoming increasingly complex. As regulations change, covered entities, including healthcare providers, health plans, and business associates, must stay informed and adaptable to meet compliance standards. Healthcare law encompasses a broad range of legal disciplines, including compliance, patient rights, protected health information (PHI), and more. Staying compliant in such a dynamic field can be a daunting challenge for hospitals, clinics, and other healthcare organizations. Understanding the latest trends in healthcare law is crucial to navigating this complex landscape and avoiding costly legal issues.
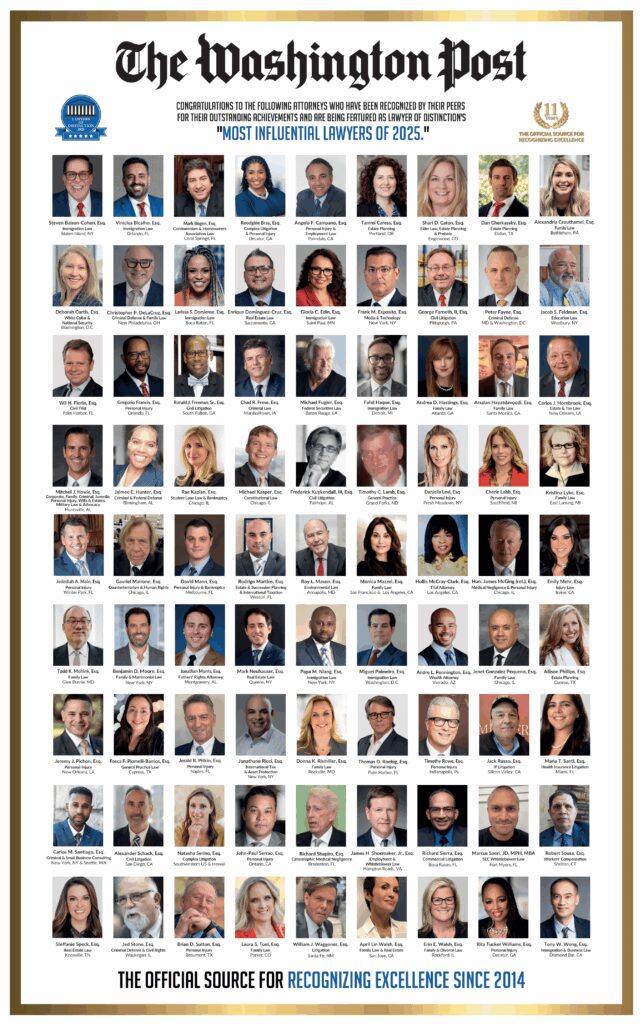
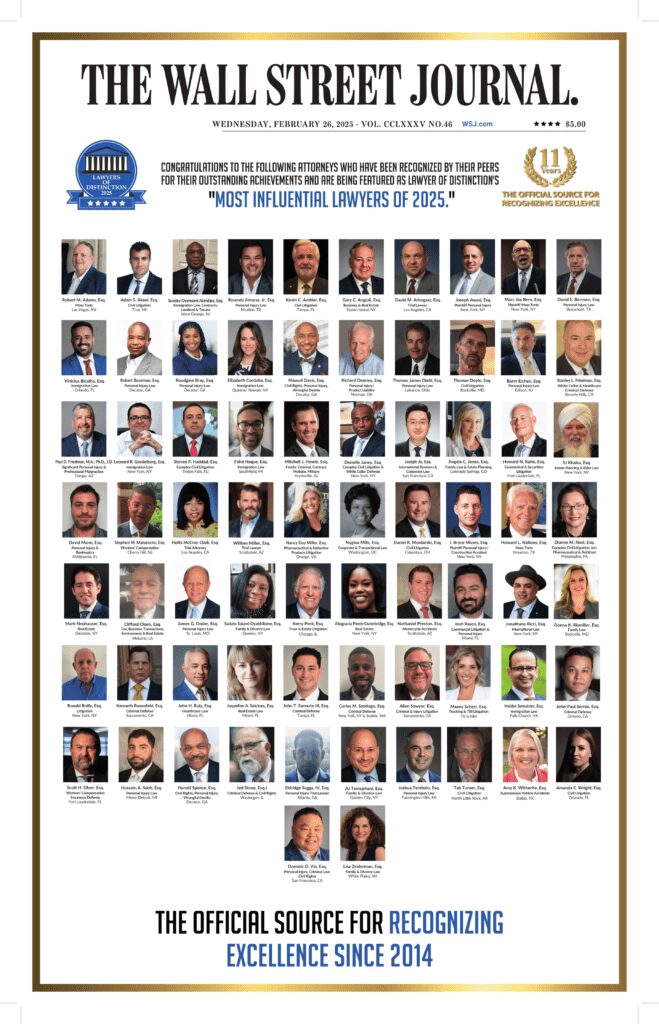
At Lawyers of Distinction (LOD), we help healthcare professionals and organizations across the nation stay ahead of regulatory changes. Our members come from all corners of the legal field, providing invaluable insights to clients needing guidance through these changes. Healthcare regulations, particularly those governed by HIPAA rules, are often confusing, and failure to comply can result in significant civil and criminal penalties. That’s where our legal expertise can help. We work alongside healthcare providers, offering solutions that ensure they meet the most current legal standards and avoid potential pitfalls.
The legal landscape in healthcare is not static—it is continually shifting. From new legislation to changes in existing regulations, healthcare law requires constant vigilance. Working with LOD’s network of legal professionals means having access to knowledge and support that can guide healthcare entities through the complexities of modern regulations.
Introduction To Healthcare Law Trends
The healthcare industry is constantly evolving, with new technologies, treatments, and regulations emerging every year. As a result, healthcare law trends are also shifting to address these changes. In this section, we will explore some of the key healthcare law trends that are shaping the industry today.
Data Privacy And Security: Adapting To Stricter Regulations
One of the most significant trends in healthcare law in recent years has been the tightening of regulations around healthcare data privacy and security. Laws such as the Health Insurance Portability and Accountability Act (HIPAA) have long governed the use and protection of individually identifiable health information. However, as technology has advanced, so have the risks associated with electronic protected health information (ePHI) breaches and identity theft. In response, lawmakers have introduced more stringent requirements to protect patient data. Healthcare providers must ensure that their systems are compliant with the latest standards or face severe fines and reputational damage.
The rise of electronic health records (EHRs) has revolutionized patient care but has also introduced new challenges in terms of data security. Healthcare organizations must now focus on safeguarding sensitive patient data to comply with healthcare compliance laws, both from potential cyberattacks and accidental disclosures. The penalties for non-compliance with HIPAA privacy rules and similar regulations can be substantial, making it essential for healthcare organizations to invest in robust data protection and security measures.
Moreover, data protection regulations are not just limited to HIPAA. In states like California, laws such as the California Consumer Privacy Act (CCPA) impose additional obligations on healthcare organizations. These laws grant patients more control over their patient data, including the right to access, delete, and move electronic health information and restrict the sharing of their medical records. As these regulations continue to evolve, healthcare providers must be vigilant in updating their privacy policies and procedures to remain compliant with national standards.
HIPAA (Health Insurance Portability and Accountability Act)
One of the most significant healthcare law trends is the continued importance of HIPAA compliance. HIPAA is a federal law that sets standards for protecting sensitive patient data, and it applies to all healthcare providers, health plans, and healthcare clearinghouses. With the rise of electronic health records (EHRs) and telemedicine, HIPAA compliance is more crucial than ever. Healthcare providers must ensure that they have robust security measures in place to protect patient data, including encryption, access controls, and secure data storage.
Telehealth Legal And The Expansion Of Virtual Care
The COVID-19 pandemic dramatically accelerated the adoption of telehealth services, which has, in turn, led to changes in healthcare law. Prior to the pandemic, the telehealth service regulations were limited, and the technology was primarily used for rural or hard-to-reach patients. However, as in-person visits became more difficult during the pandemic, telehealth services became a necessity for many providers and patients. Consequently, federal and state laws have been updated to accommodate this shift, making telehealth services more accessible.
Telehealth presents its own unique set of legal challenges. Healthcare providers must be licensed to practice in the state where the patient is located. This has led to an increased focus on cross-state licensing laws and agreements between states to recognize out-of-state medical licenses. It is crucial to understand the varying telehealth legal requirements across different states, such as consent, online prescribing, and cross-state licensing. In addition, reimbursement policies have also had to adapt, as insurance companies now cover telehealth visits in much the same way they would cover in-person visits.
As telehealth continues to grow, legal professionals expect additional regulatory changes. For instance, patient consent, data security, and privacy regulations will need to keep up with the increased use of telehealth technologies. Healthcare providers offering virtual care must ensure that their practices align with these evolving regulations to avoid legal complications.
Compliance With Emerging Payment Models
Another significant trend in healthcare law is the shift towards value-based care models. Traditionally, healthcare providers have operated on a fee-for-service basis, meaning they are paid based on the number of services provided. However, recent healthcare reforms are pushing for a model where providers are reimbursed based on patient outcomes. This shift is intended to incentivize high-quality care rather than simply more care, but it also brings new legal challenges.
Healthcare organizations must now navigate regulations related to payment models that tie compensation to the quality of care rather than the quantity. These models, including Accountable Care Organizations (ACOs) and bundled payment initiatives, have specific legal requirements that providers must understand. For example, providers must adhere to strict reporting guidelines to demonstrate improved patient outcomes.
Compliance with these new payment models often requires significant changes to the way healthcare organizations operate. Legal professionals can help providers understand their obligations under these emerging models and ensure that they remain compliant with both federal and state regulations. As these payment models continue to evolve, legal guidance will be essential in navigating the complexities of the healthcare reimbursement landscape.
The Rise Of Artificial Intelligence In Healthcare Law
Artificial intelligence (AI) is making waves in the healthcare industry, offering new tools for patient care, diagnosis, and data analysis. However, with AI comes new legal considerations, particularly in the areas of liability and compliance. As AI systems become integrated into healthcare, ensuring that they meet ethical and legal standards is a top priority for lawmakers.
One major issue with AI in healthcare is determining who is responsible for errors or harm caused by AI-driven decisions or human services. If an AI system misdiagnoses a patient or provides incorrect treatment suggestions, the question of liability becomes complex. This is an emerging area of healthcare law, and as AI continues to advance, legal frameworks will need to adapt to these new challenges.
Moreover, AI systems must comply with existing healthcare regulations, including HIPAA rules and privacy and security rules. Ensuring that AI technologies properly handle electronic patient data is crucial to maintaining compliance with data privacy laws and avoiding potential legal repercussions. Healthcare providers adopting AI for such information will need to work closely with legal professionals to ensure their systems are compliant with both existing and future regulations.
Managing Compliance In Cross-Border Healthcare Services
With the globalization of healthcare, cross-border services have become increasingly common. This trend is particularly evident in the rise of medical tourism and the growing use of telehealth platforms to treat patients across international borders. However, navigating the legal frameworks that govern cross-border healthcare services presents significant challenges for healthcare providers everywhere.
Healthcare laws and regulations vary widely from country to country, meaning that healthcare providers must be aware of the legal requirements in each jurisdiction where they offer services. In some cases, this may involve obtaining multiple licenses or complying with conflicting regulatory requirements. Ensuring that healthcare providers are compliant with the laws in all relevant jurisdictions is a complex task that requires legal expertise.
Furthermore, cross-border healthcare services raise concerns about data privacy and security. Transferring patient information across international borders can create legal complications, particularly when different countries have different privacy standards. Healthcare providers must ensure that they comply with all relevant data protection laws to avoid potential legal issues when offering cross-border health and human services elsewhere.
Healthcare Antitrust Laws: Ensuring Fair Competition
Antitrust laws are designed to prevent anti-competitive behavior and ensure that healthcare markets remain fair and competitive. With the increasing consolidation of healthcare providers, including hospital mergers and acquisitions, antitrust laws are more relevant than ever. Ensuring compliance with these laws is crucial for healthcare organizations looking to expand or merge with other entities.
Healthcare mergers can raise concerns about reduced competition, higher costs, and limited choices for patients. Regulatory agencies such as the Federal Trade Commission (FTC) closely scrutinize mergers and acquisitions in the healthcare sector to ensure they do not harm competition. Healthcare providers considering mergers must be aware of the potential legal implications and work with legal experts to navigate the antitrust approval process.
In addition to mergers, healthcare providers must also be cautious of other practices that could raise antitrust concerns, such as price-fixing or exclusive contracts. These practices can lead to legal challenges and significant penalties if they are found to violate antitrust laws. Legal guidance is essential to these regulatory concerns and ensuring that healthcare organizations remain compliant with these complex regulations.
Patient Rights And Informed Consent In Healthcare Law
Patient rights are a fundamental aspect of healthcare law, and ensuring that patients are fully informed about private health information and their treatment options is a legal requirement. Informed consent is the process by which healthcare providers must disclose all relevant information about a patient’s condition, treatment options, and potential risks. This allows patients to make informed decisions about their medical care.
Failing to obtain proper informed consent can result in legal liability for healthcare providers. If a patient suffers harm and is not fully informed about the risks of their treatment, they may have grounds for a lawsuit. Healthcare providers must ensure that they have protected patient health information (PHI) and follow strict informed consent protocols to avoid legal complications.
In addition to informed consent, patients have other rights under healthcare law, civil rights including the right to privacy, the right to access their medical records, and the right to refuse treatment. Healthcare providers must be aware of these rights and ensure that their health plans and practices comply with the HIPAA privacy rule and other legal standards governing patient rights.
Employment Law In The Healthcare Sector
Employment law plays a critical role in the healthcare sector, particularly in areas such as labor disputes, employee benefits, and workplace safety. Healthcare providers must ensure that their employment practices comply with federal and state labor laws to avoid legal challenges. This includes issues such as wage and hour laws, and employee training and classification, and the rights of healthcare workers to form unions.
Workplace safety is another important consideration in the healthcare sector. Healthcare workers are often exposed to hazardous conditions, and employers are legally obligated to provide a safe working environment. Failure to comply with Occupational Safety and Health Administration (OSHA) standards can result in significant penalties and legal liabilities for healthcare providers.
Additionally, healthcare employers must be aware of anti-discrimination laws that protect workers from unfair treatment based on factors such as race, gender, and disability. Ensuring that employment practices are fair and comply with these laws is essential to maintaining a legally compliant and ethical workplace in the healthcare sector.
Navigating Healthcare Fraud And Abuse Laws
Healthcare fraud and abuse laws are designed to prevent fraudulent activities in the healthcare system, such as billing for services not provided or providing unnecessary treatments. Laws such as the False Claims Act and the Anti-Kickback Statute impose strict penalties on healthcare providers found guilty of fraud or abuse. Ensuring compliance with these laws is critical to avoiding legal issues and maintaining the integrity of the healthcare system.
The False Claims Act enables whistleblowers to bring lawsuits on behalf of the government against healthcare providers suspected of engaging in fraudulent activities. Healthcare organizations must have robust compliance programs in place to detect and prevent fraudulent activities. Failure to comply with these laws can result in significant financial penalties and damage to a provider’s reputation.
The Anti-Kickback Statute prohibits healthcare providers from offering or receiving kickbacks in exchange for patient referrals. Violations of this law can result in criminal penalties, including fines and imprisonment. Healthcare providers must be aware of the legal restrictions on financial relationships with other healthcare providers and ensure that their practices comply with these laws.
Adapting To Changes In Prescription Drug Regulations
The pharmaceutical industry is heavily regulated, and changes in prescription drug regulations can have a significant impact on healthcare providers. Recent changes in drug pricing transparency laws, for example, require pharmaceutical companies to disclose pricing information to the public. These laws aim to make prescription drug prices more transparent and accessible to patients.
Healthcare providers must also comply with regulations governing the prescribing and dispensing of controlled substances. The opioid crisis has led to increased scrutiny of prescription drug practices, and healthcare providers must ensure that they follow strict guidelines to avoid legal complications. This includes proper documentation of prescriptions and compliance with state and federal laws regarding controlled substances.
Furthermore, healthcare providers must stay informed about changes in drug approval processes and the availability of new treatments. Working with legal professionals can help healthcare providers navigate the complex regulatory environment surrounding prescription drugs and ensure that they remain compliant with all relevant laws.
Corporate Practice of Medicine: Legal Considerations for Healthcare Businesses
The corporate practice of medicine doctrine restricts non-physicians and business associates from owning or controlling medical practices. This legal principle is designed to protect the integrity of the doctor-patient relationship by ensuring that medical decisions are made by qualified healthcare professionals, rather than business entities. However, corporate practice of medicine laws vary from state to state, creating legal challenges for healthcare businesses.
In some states, healthcare businesses are prohibited from employing physicians directly, while in others, healthcare entities can own and operate medical practices under certain conditions. Healthcare providers must be aware of the corporate practice of medicine laws in their state and ensure that their business structures comply with these regulations.
Failure to comply with the corporate practice of medicine laws can result in legal penalties, including the loss of a full medical practice or license. Healthcare providers and businesses must work with legal professionals to ensure that their organizational structures align with the legal requirements in their state.
The Role Of Ethics Committees In Healthcare Law
Ethics committees play a vital role in healthcare organizations, providing guidance on complex ethical and legal decisions. These committees are composed of healthcare professionals, ethicists, and legal experts who collaborate to address ethical dilemmas, such as end-of-life care, patient autonomy, and informed consent. Ethics committees are especially important in navigating situations where legal obligations and ethical principles may conflict.
For instance, when dealing with end-of-life decisions or cases involving patients unable to make their own medical decisions, ethics committees provide an essential layer of oversight and advice. By having legal experts involved, healthcare organizations ensure that any decisions made are compliant with both legal standards and ethical norms. Ethics committees also assist in interpreting legislation, such as healthcare directives and living wills, to align them with patient wishes and legal requirements.
The evolving landscape of healthcare law means that ethical considerations are continuously influenced by new regulations and trends healthcare and societal values. For healthcare organizations, maintaining a strong and active ethics committee ensures that complex legal and ethical issues are handled in a compliant and compassionate manner.
Medical Malpractice Laws: Protecting Patients And Providers
Medical malpractice laws exist to hold healthcare providers accountable for negligence that harms patients, but these laws also protect providers from frivolous lawsuits. Legal protections vary from state to state, but the core of medical malpractice law is ensuring that patients receive fair compensation for harm caused by medical errors while also ensuring that healthcare providers can defend themselves against unfounded claims.
For healthcare providers, staying informed about malpractice laws and regularly reviewing their practices is critical to avoiding litigation. Legal professionals can help providers by ensuring their documentation, procedures, and policies are up to date with local and federal regulations, thereby minimizing legal exposure. Providers who adhere to legal guidelines can better protect themselves from legal challenges and maintain patient trust.
On the other hand, patients rely on medical malpractice laws to ensure they receive compensation when healthcare providers fail to meet the standard of healthcare itself. Healthcare providers should work closely with legal experts to not only defend against malpractice claims but also prevent issues through rigorous compliance and ethical patient care.
How Technology Is Shaping Compliance In Healthcare Law
Technology is transforming the way healthcare organizations ensure compliance with laws and regulations. From electronic health records (EHRs) to telehealth platforms, technology helps streamline administrative tasks, improve patient care, and track compliance in real time. However, the integration of technology into healthcare has also introduced new legal challenges, particularly related to privacy, data security, and liability.
One of the main advantages of technology in healthcare compliance is the ability to track and audit operations more efficiently. Compliance software allows healthcare providers to monitor and ensure that their practices meet legal standards in areas such as patient privacy, billing, and employee safety. This real-time monitoring helps identify potential legal issues before they escalate into violations or litigation.
However, healthcare organizations must ensure that the technology they adopt complies with all relevant laws, including HIPAA compliance and data privacy regulations. The improper use of technology can lead to data breaches and legal liabilities, making it essential for healthcare providers to work with legal professionals when implementing new technologies.
Why Choose Lawyers Of Distinction For Your Healthcare Law Needs?
At Lawyers of Distinction, we recognize the immense challenges healthcare providers face when dealing with rapidly changing regulations. Our members are leaders in healthcare law, offering valuable insights and expert legal services to help healthcare organizations stay compliant with the latest legal trends. Whether it’s ensuring data privacy, adapting to telehealth regulations, or navigating value-based care models, LOD provides comprehensive support to meet your needs.
We offer a nationwide network of experienced attorneys who understand the intricacies of healthcare law. Our legal experts are not only knowledgeable in federal regulations but are also well-versed in state-specific laws, ensuring that you receive tailored advice that fits your organization’s unique situation. To learn more about how we can help, visit our website or reach out through our contact form at Lawyers of Distinction Contact or call us at (877) 335-3021 for a consultation today.